- 1School of Psychology, The University of Sheffield, Sheffield, United Kingdom
- 2Nestlé Purina PetCare, Barcelona, Spain
- 3Mind Field Advertising, Manchester, United Kingdom
- 4Perfect Circle, Manchester, United Kingdom
- 5Companion Consultancy, Littleborough, United Kingdom
Introduction: Obesity is a serious and prevalent problem in dogs. The causes are multifactorial, but owners play a key role and so this paper reports the development and evaluation of a health pack designed to help owners to manage the weight of their dogs.
Method: The pack was informed by previous research, behavior change theory (i.e., the COM-B model), and interviews with 12 veterinary professionals to identify challenges and potential solutions. Six workshops with a total of 28 dog owners provided feedback on the initial ideas. The pack included information on the importance of weight management, how to weigh and assess body condition score (BCS), a journal to track progress, an infographic illustrating the calorific value of treats, cards to help owners manage difficult situations, and a collar tag for the dog. The acceptability of the materials and potential outcomes were evaluated in a pre-registered pilot trial with a sample of 78 dog owners who were posted a health pack, 49 of whom completed a follow-up questionnaire.
Results: The findings suggested that owners were willing to weigh their dog, found the pack acceptable, and there was preliminary evidence that the weight and BCS of dogs was lower at follow-up than at baseline.
Discussion: The findings illustrate the potential of a health pack for supporting dog owners and provide the basis for a larger RCT to formally evaluate effectiveness.
1 Introduction
Obesity among companion animals is a serious and increasingly common problem. The prevalence of canine obesity ranges between 25 and 44% in developed countries (1) and, according to the results of the Pet Obesity Survey (2), the prevalence of obesity is increasing. Obesity is a medical condition characterized by the accumulation of excess body fat to a degree that can adversely impact health (3). Rather than being a passive tissue, excessive body fat is recognized to have far-reaching effects on various organ systems through inflammatory, neuroendocrine, and other mechanisms. Overweight dogs are particularly susceptible to a range of health issues, including metabolic, endocrine, renal, urinary, respiratory, orthopaedic, dermatological, neoplastic, and ophthalmologic conditions (4–7). These animals often experience a diminished quality of life (8–10) and have shorter lifespans, with evidence that obese dogs die on average 1–2 years earlier than their non-obese counterparts (11–12). Therefore, identifying ways to detect, prevent, and manage obesity in companion animals is critical.
Risk factors for obesity among companion dogs are multifactorial and include factors pertaining to the dog (e.g., genetics, breed, neutered status, age, sex, responsiveness to food, and diseases like diabetes mellitus or hypothyroidism) (7, 13, 14). However, owners typically control food intake and can moderate energy expenditure among companion animals, which has led some to advocate for a behavioral science approach to managing obesity among companion animals that focuses on the owner, rather than – or in addition to – their dog (15, 16). A number of factors related to the owner have been shown to be associated with overfeeding and poor weight outcomes, including not realising that the dog is overweight (17, 18), not appreciating the risks of obesity (19) or associating costs with dog ownership (20), owners’ levels of physical (in)activity (21), using food as a way to bond with the dog (22), allowing the dog to be present when preparing or eating food (23) and excessive use of treats (24, 25).
While research is making progress identifying the factors that influence the way that owners feed and exercise their companion animals, less research has translated these insights into practical and acceptable interventions that can support owners to make changes to their behavior. There are examples of successful weight loss programmes, but these typically focus primarily on caloric restriction or other dietary changes and are implemented in controlled environments (26–29). Outside such controlled environments, veterinary professionals try to advise and support owners [e.g., via nurse-led clinics (30, 31)]. However, there is limited time in such consultations, veterinary professionals may find discussing obesity challenging (32–35), owners may dismiss or struggle to follow advice (36), and recommendations may not translate into the owner’s home environment (37). Indeed, interventions delivered outside the laboratory are often associated with relatively low levels of compliance (38, 39). For example, German et al. (40) found that only around 60% of dogs referred to a controlled feeding programme completed the programme. Reasons for stopping prematurely included refusal to comply with weight management advice.
Taken together, there is a clear need for an intervention that can support owners to make changes to their behavior - and perhaps support veterinary professionals to work with owners to do so. Interventions have targeted owners’ behavior. For example, a review by Krasuska and Webb (41) identified 14 interventions targeting owners’ behavior. However, with a few notable exceptions that examined the effect of monthly classes on nutrition (42) and collaborative exercise programs (43–45), the majority of the studies simply recommended that owners feed less or differently but provided little or no support for so doing (46). Other interventions required access to specialist equipment [e.g., an underwater treadmill (47)]. Webb et al. (48) tried to support owners by developing a volitional help sheet (49) designed to help owners to form if-then plans specifying how to deal with challenging situations (e.g., ‘If my dog is begging for a treat, then I will give him/her a cuddle instead!’). Over 600 studies support the idea that this type of planning [known as ‘implementation intentions’ (50)] helps people to achieve their goals (51); yet Webb et al. (48) found no difference in the behavior of owners in the intervention condition and those in the control condition who did not receive the help sheet. One reason was that the helpsheet was embedded at the end of a relatively long questionnaire and less than half of the sample completed the planning exercise.
This example points to the importance of ensuring that interventions are acceptable to those who are expected to engage with and use them. Acceptability refers to the extent to which people receiving the intervention consider it to be appropriate, based on anticipated or experienced cognitive and emotional responses to the intervention (52). Acceptability has become a key consideration in the design, evaluation and implementation of healthcare interventions (52), but seems to be rarely considered in preventive veterinary medicine, despite evidence that compliance with advice and interventions is often low (38–40) and that owners may not believe that recommendations are acceptable. For example, MacMartin et al. (36) reported that owners found nutritional suggestions made by veterinarians potentially unnecessary, inappropriate, or unfeasible. Acceptability is a necessary precondition for an intervention to be effective and the reason why those developing interventions – including the present team – view an ‘acceptability trial’ as critical. We need to know that owners are willing to use an intervention before we can assess whether the components of the intervention influence outcomes.
Evidence suggests that interventions that are based on theory are typically more effective than those that are not and theory can provide a framework for developing interventions (53). The COM-B model developed by Michie et al. (54) is one of the most influential frameworks for understanding behavior and developing interventions. The model suggests that three components are needed for any behavior to occur. First, the person must be motivated; that is, they must want, or appreciate the need, to behave in a certain way (e.g., take steps to change the way that they feed their dog because they recognise that their dog is overweight and appreciate the risks of being overweight). However, the COM-B model recognises that motivation alone is unlikely to lead to changes in behavior [cf. research on the gap between intentions and behavior (55–56)] and therefore proposes that the person must also be capable and have the opportunity to act. Capability refers to whether the person has the physical strength, knowledge, skills, stamina etc. to perform the behavior (e.g., an owner who does not know when, what, or how much to feed their dog is unlikely to be able to feed appropriately (48)). Opportunity reflects the need for a conducive physical and social environment for behavior (e.g., an owner needs a measuring cup or small set of scales in order to feed an appropriate amount of food). The COM-B model has been used to develop a wide range of interventions, including in veterinary science [e.g., to understand behaviors such as disease control among cattle farmers (57–59) and obesity among horses (60)]. It therefore has the potential to provide a useful framework for understanding dog owners’ behavior and informing the design of an intervention designed to support changes where needed.
The aim of the proposed research was to develop a health package that will support owners to change their behavior and reduce weight among companion animals. The preceding discussion suggests that interventions need to draw on theoretical frameworks and insights from behavioral science - yet also be developed alongside owners to ensure that they are accessible and acceptable. The research therefore involved two phases – (i) a development phase and (ii) evaluation of acceptability and preliminary evaluation of effects on potential outcomes, including owners’ behavior and weight of their companion animals.
2 Phase 1: development
Understanding from current evidence (e.g., that reviewed in the introduction) was supplemented with interviews with veterinary professionals to identify key issues that owners encounter managing the weight of their dogs and potential strategies for supporting owners. This information was then used to compile an initial set of tools for the health pack. These initial tools were mapped to COM-B components to ensure that they targeted all of the theoretical determinants of behavior (i.e., capability, opportunity, and motivation) and were then presented to owners via a series of collaborative workshops to obtain feedback. The tools were then refined with the support of a marketing agency to create the final health pack.
2.1 Interviews with veterinary professionals
2.1.1 Materials and method
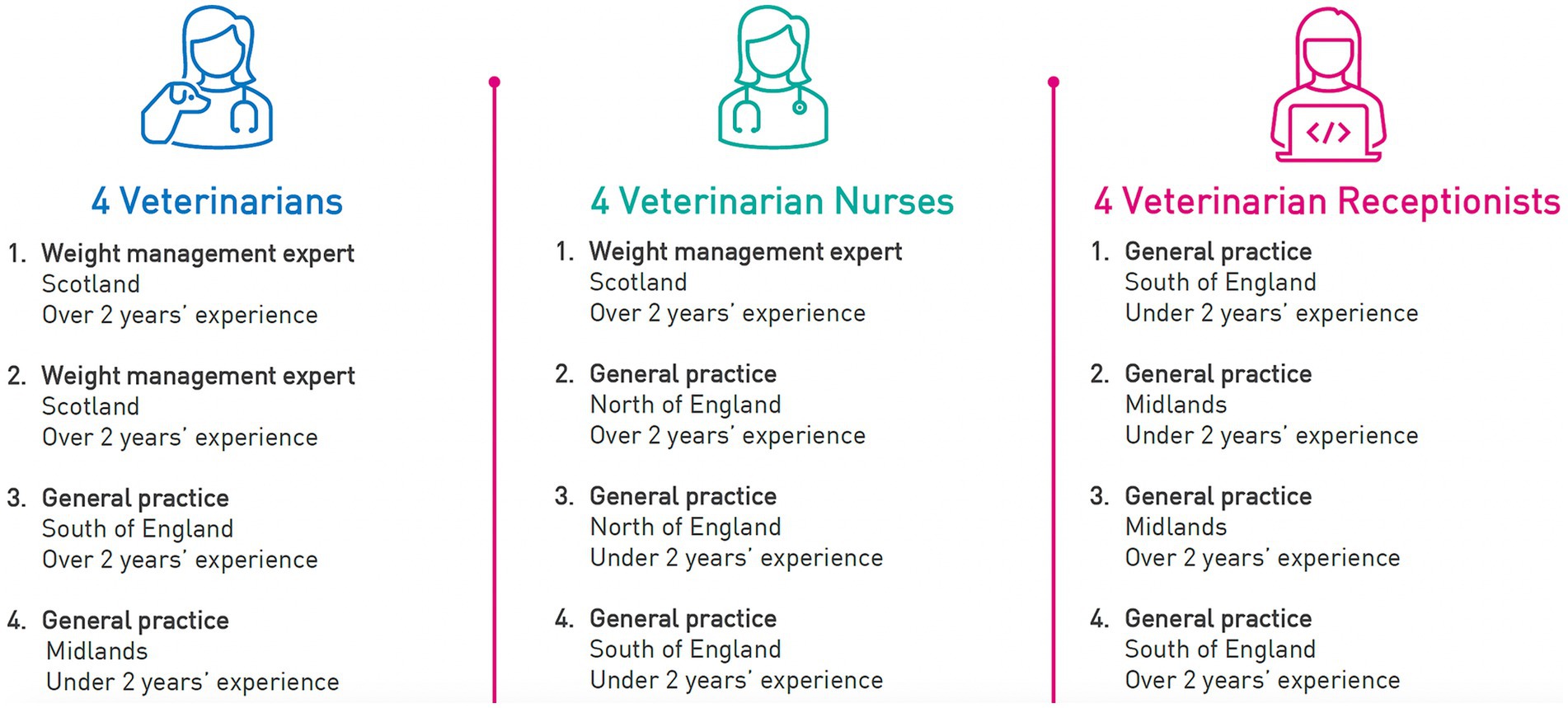
Semi-structured interviews were conducted with 12 veterinary professionals (4 veterinarians, 4 veterinary nurses, and 4 veterinary receptionists1) who worked at or owned a general veterinary practice that serves dogs. The professionals were recruited by the 5th author from a database held by Central Fieldwork and were selected to represent a range of geographical regions in the UK and experience – in veterinary practice and in weight management. Figure 1 shows the characteristics of the participants in this phase of the research.
Each interview focused on the professionals’ experience of how owners manage obesity, including the issues that owners face and the strategies that the owners and veterinary practices employ to address these issues (see Supplementary Material 14.1 for the full interview guide). The interviews were recorded and analyzed to identify common themes, which were categorized into those relating to motivation, capability and / or opportunity using the COM-B model as a framework.
2.1.2 Results
The professionals identified a range of reasons that they believed led dogs to become overweight (see Table 1). The issues reflected all of the COM-B components including psychological capability (e.g., knowing how to monitor weight and intake), physical capability (e.g., the owner’s own capacity to exercise), social opportunity (e.g., family norms around feeding), physical opportunity (e.g., reduced engagement with veterinary professionals), reflective motivation (e.g., not giving sufficient attention to preventive care), and automatic motivation (e.g., humanization of companion animals).
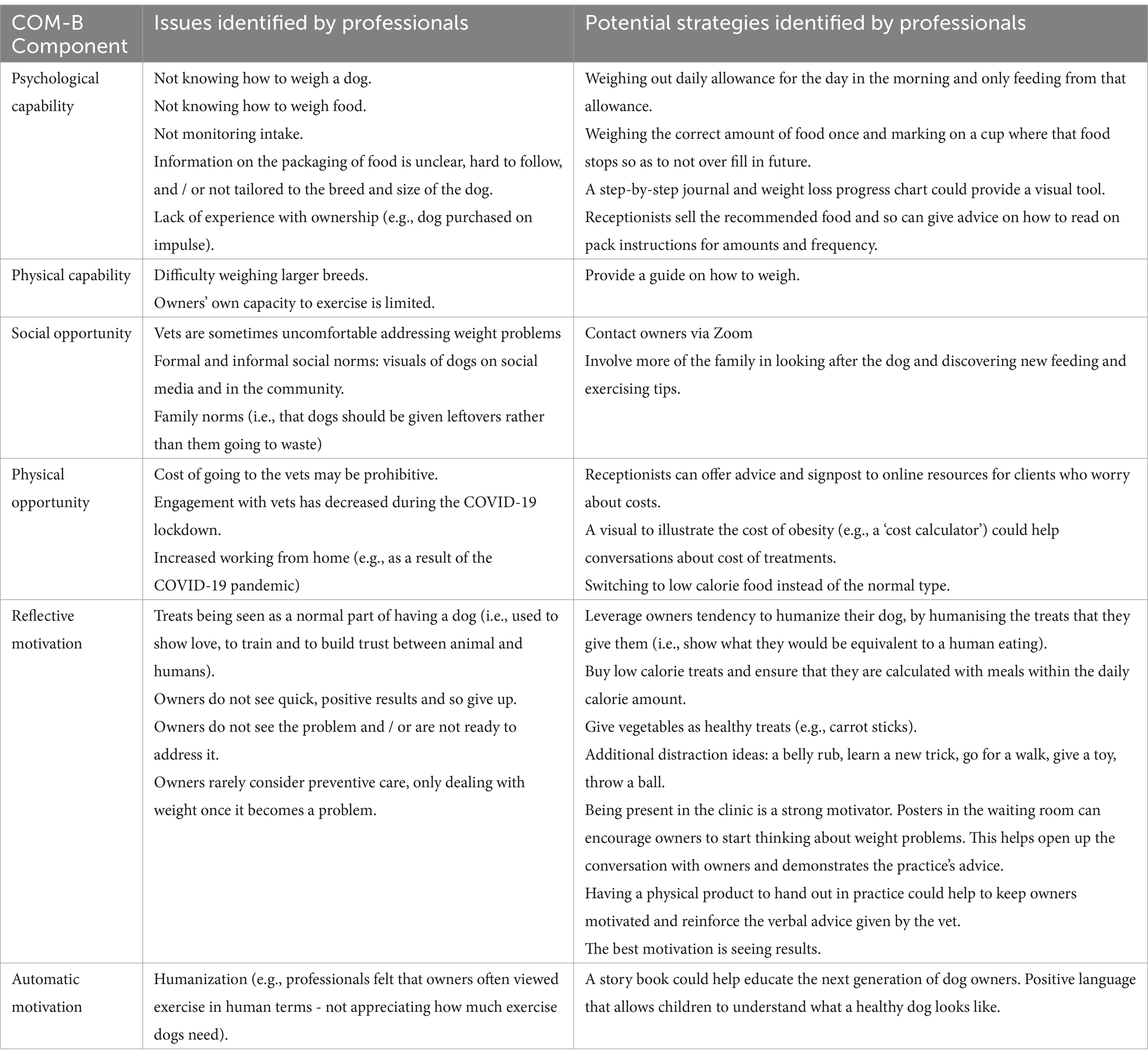
Table 1. Issues and strategies identified by veterinary professionals for managing obesity, categorized by COM-B component.
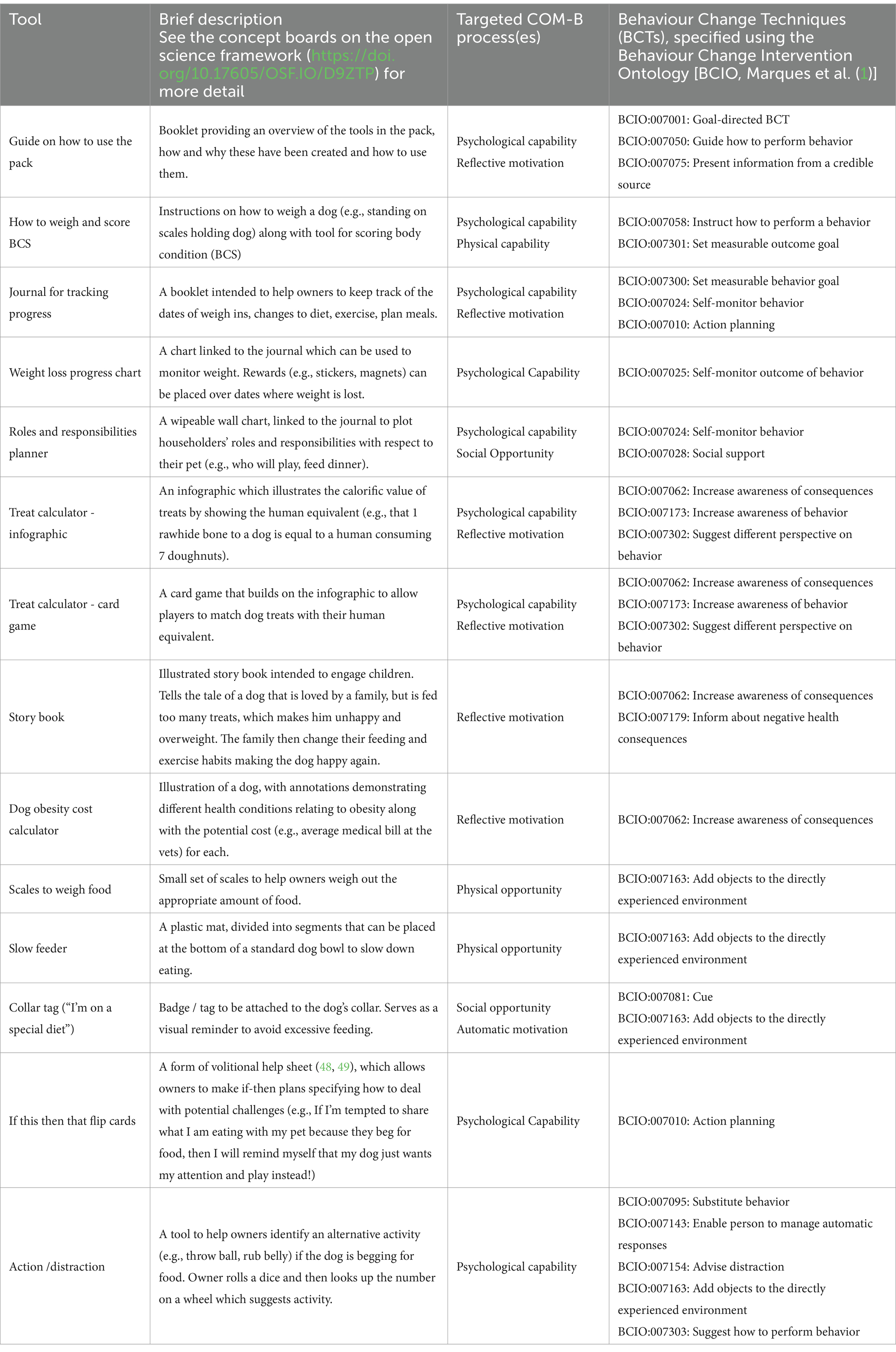
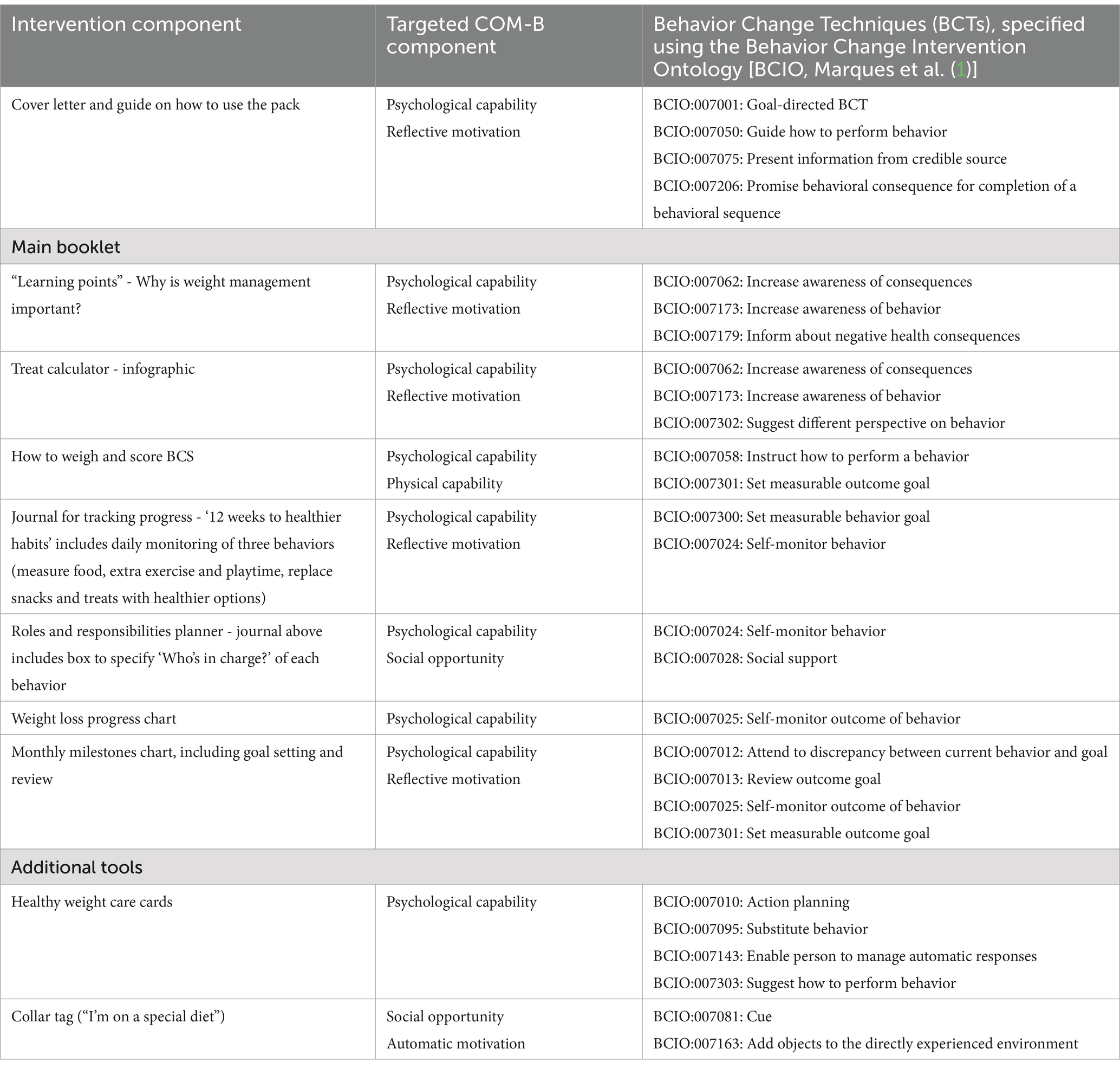
The research team then used the feedback from the professionals alongside insights from research on obesity among companion animals to develop an initial set of tools to support owners (see Table 2 for a summary). These tools were designed to target each of the determinants of behavior specified by the COM-B model (i.e., capability, opportunity, and motivation) and described in terms of the behavior change techniques [the smallest parts of an intervention that are observable, replicable, and on their own have the potential to bring about behavior change (54)] that they employed (specified using the Behavior Change Technique Ontology (61)). Using standardized frameworks to describe the content of behavioral interventions provides transparency, allows replication, and the accumulation of evidence about the effectiveness of interventions (68).
2.2 Collaborative workshops with dog owners
2.2.1 Materials and methods
Feedback on the initial set of tools was obtained from dog owners via a series of collaborative workshops. Ethical approval was granted by the Research Ethics Committee at the University of Sheffield (application #044619). Participants were recruited by the 5th author from a database held by Central Fieldwork. Potential participants were asked to complete a screening questionnaire from which owners who described having at least one dog that they deemed overweight were identified.2
Six workshops were conducted with 28 dog owners (9 male and 19 female) in three cities in the UK (Leeds, Nottingham, and Watford) in February 2022. Four of the owners (14%) did not have children, 18 (64%) had children living at home, and 6 owners (21%) had children who had left home. In terms of ethnicity, the majority of the sample (26 participants, 93%) were White British. Seventeen of the participants (61%) had 1 dog in the home and 11 of the participants (39%) had 2 or more dogs. Eleven of the participants (39%) had a small dog, 12 (43%) had a medium-sized dog and 5 (18%) had a large breed of dog. Sixteen of the participants (57%) described their dog as overweight, 2 (7%) as quite overweight and 10 (36%) as very overweight.
On arrival at the workshop, participants received information about the research, provided informed consent and were told that they would receive £70 for taking part. Each workshop lasted around 90 min and involved participants introducing themselves, saying a bit about their dog, as well as whether and how they manage the weight of their dog. The main part of the workshop involved showing participants visuals of the initial set of tools for the health pack on large ‘concept’ boards (these can be viewed on the Open Science Framework https://doi.org/10.17605/OSF.IO/D9ZTP). The moderator introduced each board and then asked participants to walk around (in pairs or small groups if wanted) and use Post-it notes to indicate (i) what they liked and why (green Post-it notes), (ii) what they did not like and why (red Post-it notes), and (iii) how they would improve it (yellow Post-it notes). Participants were then asked to share their feedback with the group and to discuss and decide which tools they felt would be most effective in helping owners to manage their dog’s weight. Finally, participants were asked to think about their personal circumstances (e.g., lifestyle, work pattern, household members) and the needs of their dog in particular and to use purple Post-it notes to identify (i) which of the tools they would see being used in their household, (ii) how they would be used and by who, and (iii) how they would help to change what they do now.
2.2.2 Results
Table 3 provides a summary of owners’ feedback on the initial set of tools. This feedback was used in a series of meetings with a marketing agency to develop and refine the tools and decide which to take forward into the final pack. It was decided to retain the guide on how to use the pack (split into a cover letter and booklet), how to weigh and score BCS, the journal for tracking progress, the roles and responsibilities planner (which became a box prompting owners to reflect on ‘who’s in charge’ of each of the three behaviors specified in the journal for tracking progress), the weight loss progress chart (which became referred to as the ‘weekly weight tracker’), the treat calculator infographic, collar tag, and the action / distraction tool in the form of ‘healthy weight care cards’. We removed the treat calculator card game, story book, dog obesity cost calculator, scales to weigh food, slow feeder, and the ‘if this, then that’ flip cards. We also added learning points (explaining why weight management is important) and a monthly milestones chart (in addition to weekly monitoring of weight) that included goal setting and review.
Table 4 provides an overview of the final set of intervention components alongside (i) the component of the COM-B model that they target and (ii) the Behavior Change Techniques [BCTs (61)] that they use to do so, specified using the Behavior Change Intervention Ontology [BCIO (62)].
3 Phase 2: evaluation
The second phase of the research sought to evaluate the acceptability of the health pack and its potential to support owners. This research should therefore be considered the ‘pilot or feasibility phase’ ahead of the ‘evaluation’ and ‘implementation’ phases (52) and was not intended to evaluate whether receipt / use of the pack leads to changes in behavior and / or outcomes for the companion animal (although we measured these things, the study did not randomise participants to condition, nor did it have sufficient statistical power to detect changes over time). The evaluation of the health pack and hypotheses below were pre-registered on the Open Science Framework (https://osf.io/e65wj).
3.1 Hypotheses
Primary hypotheses.
1. Owners will be willing and able to self-assess and report their dog’s weight3 and Body Condition Score (BCS).
2. Owners who are posted a health pack will report using that pack.
3. Owners will find the health pack acceptable, as evidenced by agreement with items reflecting (i) affective attitudes, (ii) perceived effectiveness, (iii) intervention coherence, and (iv) self-efficacy, and disagreement with items reflecting (i) burden, (ii) ethicality, and (iii) opportunity costs.
Secondary hypotheses.
4. Owners who are posted a health pack will report (i) changing the way that they feed, exercise, or interact with their dog over the 8 weeks following receipt of the pack, and (ii) these changes will be the result of receiving or using the health pack.
5. The weight and BCS of dogs will be lower at follow-up than at baseline.
3.2 Materials and method
Ethical approval was granted by the Research Ethics Committee at the University of Sheffield (application #055570) and the internal ethics committee at Purina PetCare.
3.2.1 Participants
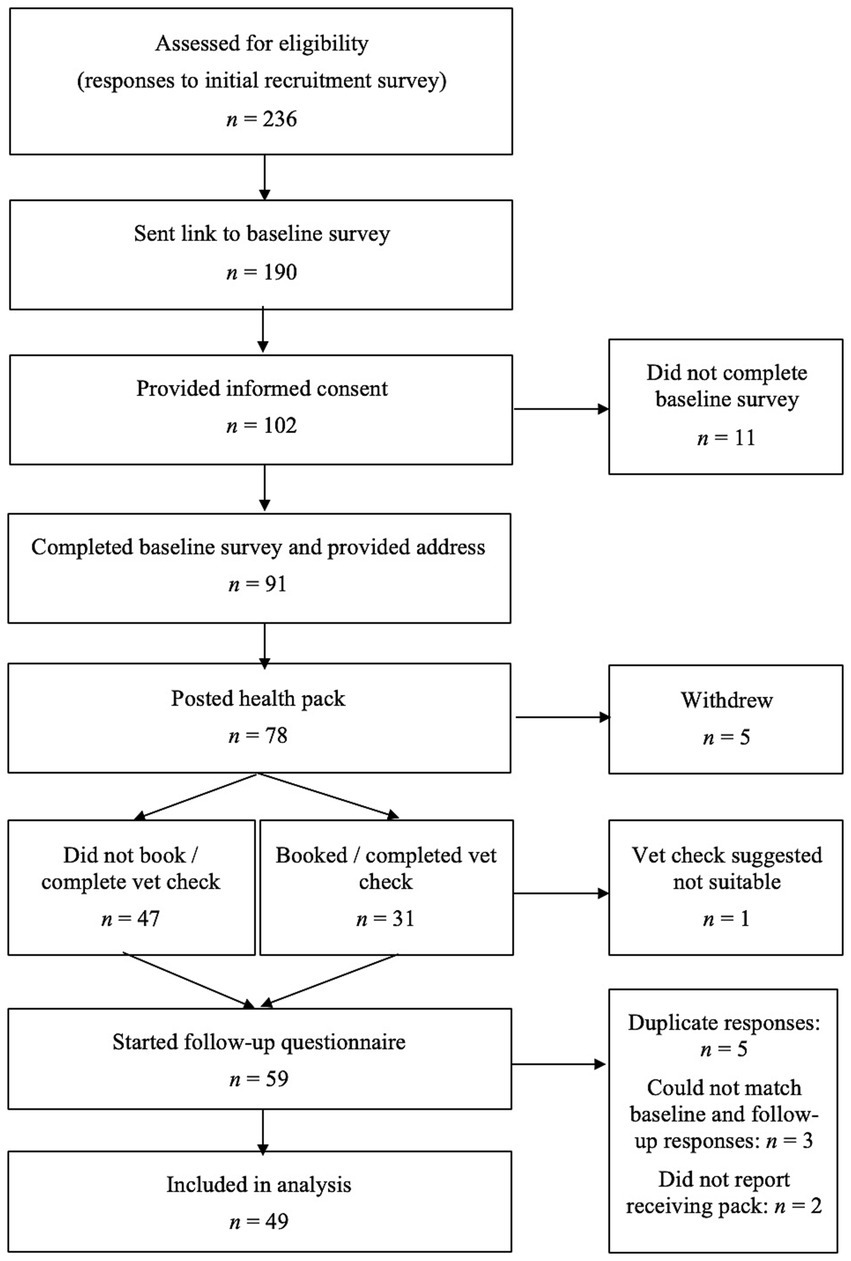
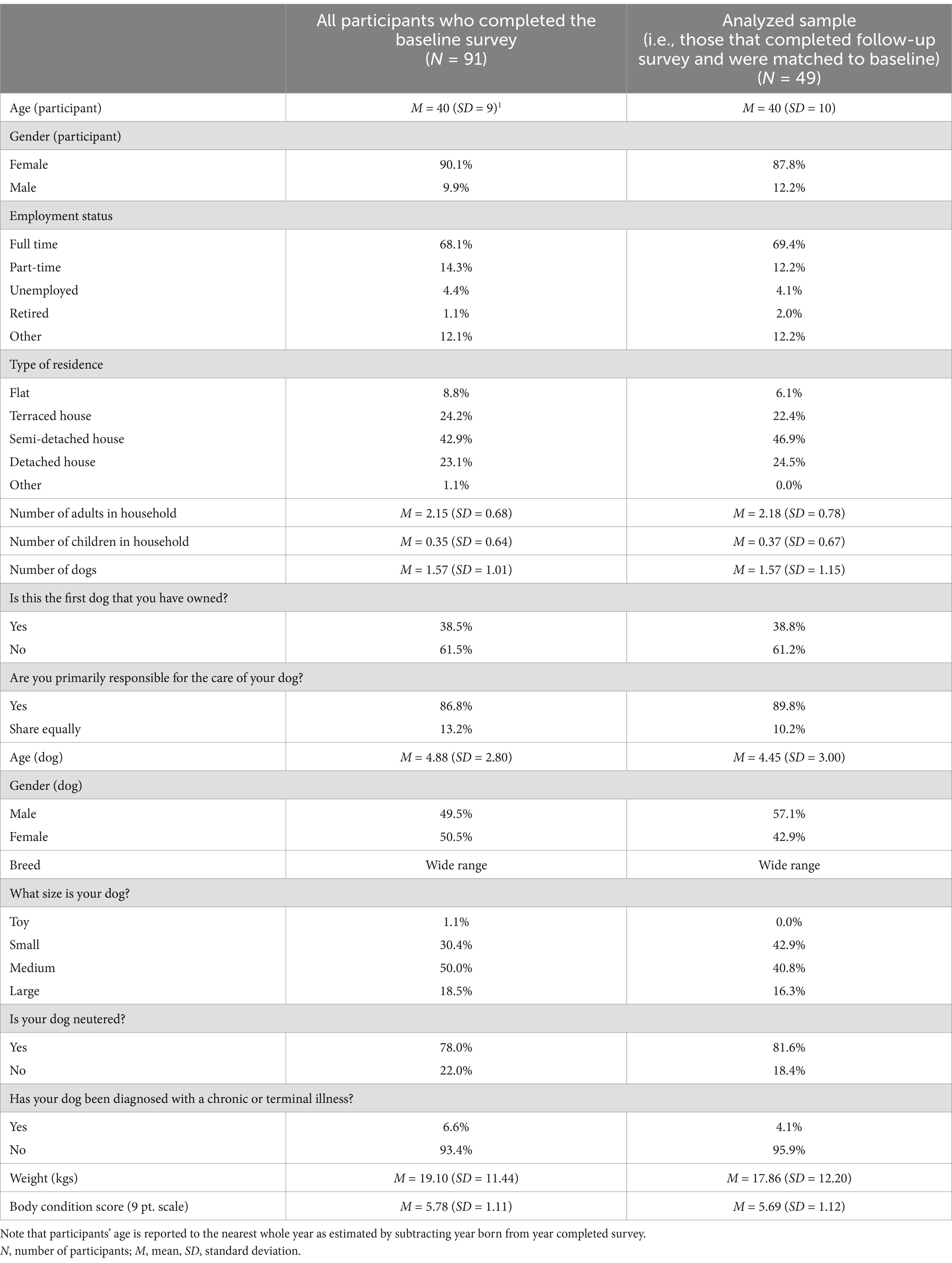
There are few criteria for identifying the sample size needed to investigate the acceptability of an intervention and previous studies with relatively small samples have been highly cited. For example, Ben-Zeev et al. (63) recruited 33 participants to assess the acceptability of a smartphone intervention for schizophrenia. We therefore decided to aim for 50 participants with complete data (i.e., completed pre- and follow-up measures) and to recruit up to 80 participants, assuming that not all would complete the follow-up measures. Owners of overweight dogs were recruited using a snowball recruitment method, starting with owners in the UK that were known to the recruitment agency and via an advert posted on Facebook, Instagram and LinkedIn and in local places across the UK. The sample did not include owners who had taken part in the research used to develop the pack. Owners were not incentivized to complete the initial questionnaire or use the toolkit, but were told that they would receive a small incentive (£25) for answering the second questionnaire. Figure 2 shows the flow of participants through the study and Table 5 shows the characteristics of participants at baseline.
3.2.2 Procedure
3.2.2.1 Initial questionnaire
Owners were contacted by email and asked to complete an initial questionnaire designed to obtain information about them, their household, and their dog, including: (i) their age and gender, (ii) employment status, (iii) type of housing (e.g., flat, terrace, semi-detached, detached), (iv) household composition (number of adults, number of children), (v) age and gender of dog, (vi) breed of dog, (vii) size of dog, (viii) neutered status, (ix) whether they are the primary carer, (x) whether the dog has been diagnosed with a chronic or terminal illness, (xi) weight of dog (if known), and (xii) self-assessed Body Condition Score (BCS) on a 9-point scale.4
3.2.2.2 Health pack
At the end of the initial questionnaire, participants were asked to provide their name and address. We then posted them the health pack designed to help them to manage the weight of their dogs. On receipt of the pack owners were asked to schedule a complimentary online call with a vet (the last author, SM), primarily to check that their dog is healthy and to provide a preliminary evaluation of BCS. However, this call also sought to agree goals for the trial. Specifically, for dogs with a BCS of 6 or above, it was suggested that owners reduce the amount of food they provide by 10% for the duration of the trial (BCIO:007004: Agree behavior goal). Some guidance on the ideal weight for their dog was also provided (BCIO:007006: Agree outcome goal).
3.2.2.3 Follow-up questionnaire
Around ten weeks (M = 68 days, SD = 7, range: 62 to 92 days) after the pack was posted to owners, they were contacted by email a second time and asked to complete a second questionnaire designed to measure their views of the pack.5 On average, participants completed the follow-up questionnaire 85 days after the baseline questionnaire (SD = 18, range: 64 to 155 days).
Participants were first asked whether they (and / or members of their household) had used the pack. If so, participants were asked which tools they had used and how. If not, participants were asked why they (or others in their household) had not read or used any parts of the pack. Participants then completed measures of the seven components of acceptability delineated by Sekohn et al. (52): (i) affective attitude, (ii) burden, (iii) perceived effectiveness, (iv) ethicality (the extent to which the intervention has good fit with an individual’s value system), (v) intervention coherence, (vi) opportunity costs, and (vii) self-efficacy. Each component was measured by asking participants to respond to a series of statements on a 5-point scale.
Affective attitude was measured with two items: “I liked using the health pack” and “I enjoyed using the health pack.” These items proved internally reliable (Cronbach’s alpha = 0.83) and were combined into a single index.
Burden was measured with one item: “How much effort did it take to use the health pack?”
Perceived effectiveness was measured with three items: “Using the health pack helped me to manage my dog’s weight,” “The health pack helped me talk to my vet / vet nurse about how to manage my dog’s weight,” and “The health pack would support a range of different owners to manage their dog’s weight if needed.” These items proved internally reliable (Cronbach’s alpha = 0.76) and were combined into a single index.
Ethicality was measured with four items: “It is okay to put a dog on a diet,” “It is wrong to limit the amount of food given to a pet” (recoded), “Using the health pack made me feel like I was being kind to my dog,” and “Using the health pack made it difficult to show that I love my dog” (recoded). These items did not prove internally reliable (Cronbach’s alpha = 0.50) and the reliability could not be improved by removing items. Therefore, the items were considered individually in the analyses.
Intervention coherence was measured with one item: “It was clear to me how using the health pack could help me to manage my dog’s weight.”
Opportunity costs were measured with two items: “Using the health pack interfered with my other priorities” and “Using the health pack made looking after my dog a chore.” These items were deemed sufficiently reliable (Cronbach’s alpha = 0.67) to combine into a single index.
Self-efficacy was measured with two items: “How confident did you feel about using the health pack?” and “I found it easy to use the health pack to manage my dog’s weight.” These items did not prove internally reliable (Cronbach’s alpha = 0.37), which suggested that they reflected slightly different beliefs. Therefore, the items were considered individually in the analyses.
The follow-up questionnaire also asked participants about their behavior (“Have you (or those in your household) changed the way that you feed, exercise, or interact with your dog over the last 8 weeks?”). If owners reported changing their behavior, they were asked to specify how their behavior had changed (we categorized owners’ responses as reflecting changes in feeding behavior, exercise behavior and / or interaction with the dog) and whether any changes in behavior were the result of using the health pack (“Were any of these changes the result of receiving or using the health pack?”) or something else (“Please let us know if anything has happened over the last 8 weeks that has affected you or your dog”). Finally, owners reported whether they had recently weighed their dog (and, if so, what it weighed) and self-assessed their dog’s BCS, again on a 9-point scale.
4 Results
All statistical analyses were conducted using SPSS (version 29 for Mac).
4.1 Hypothesis 1: owners will be willing and able to self-assess and report their dog’s weight and body condition score (BCS)
Our pre-registered criteria for inferring Hypothesis 1 to be supported was that more than 70% of the owners who completed the follow-up questionnaire would report their dog’s weight and BCS. Of the 91 of the participants who completed the baseline survey, 89 (98%) reported their dog’s BCS and 80 (88%) reported that they knew how much their dog weighed, suggesting that in general, owners were willing and able to self-assess and report their dog’s weight and BCS. On average, the dogs owned by participants who completed the baseline survey were overweight (Mean BCS = 5.79, SD = 1.11), weighing an average of 19.10kgs (SD = 11.44).6
4.2 Hypothesis 2: owners who are posted a health pack will report using that pack
Our pre-registered criteria for inferring Hypothesis 2 to be supported was that more than 70% of the owners who were posted a health pack report would report using that pack. This hypothesis was supported on the basis that 46 of the 49 participants (94%) who were posted a health pack and completed the follow-up questionnaire reported that they (and / or other members of their household) read or used parts of the pack.
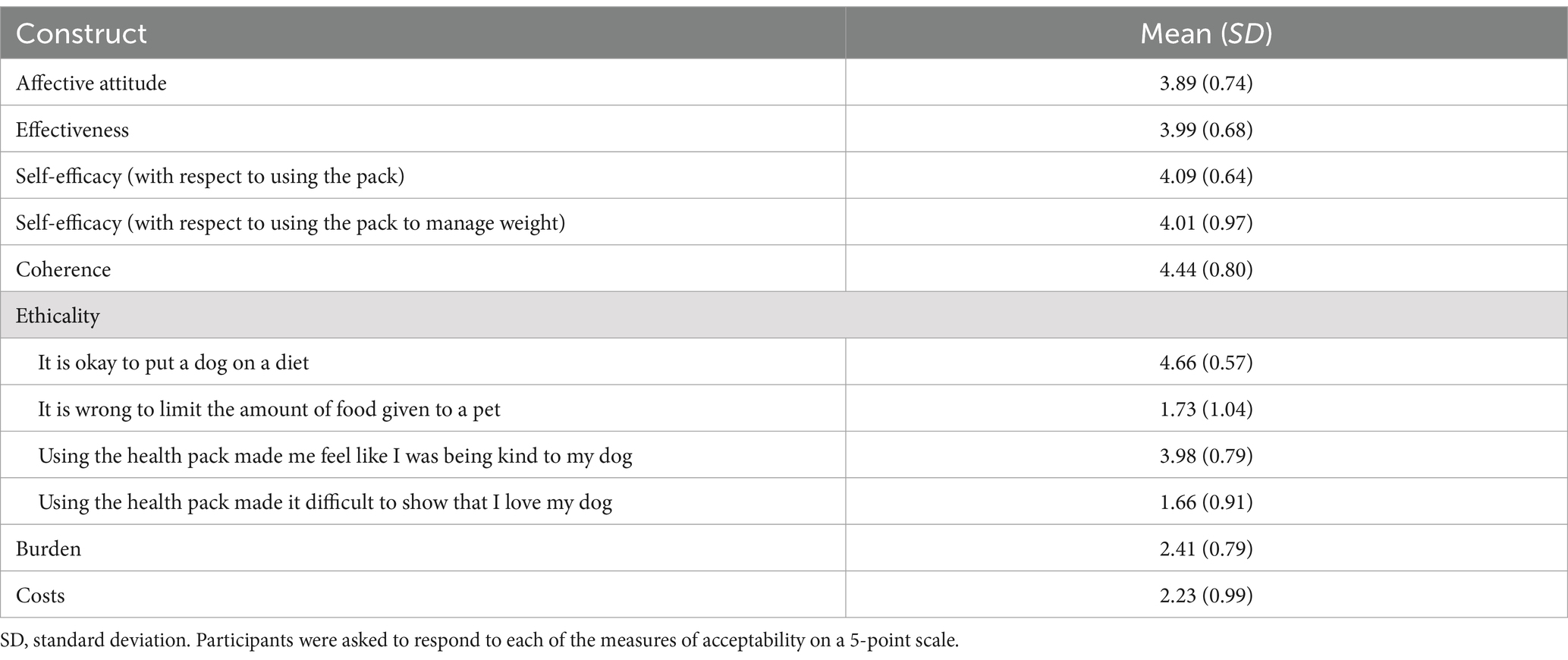
4.3 Hypothesis 3: owners will find the health pack acceptable, as evidenced by agreement with items reflecting (i) affective attitudes, (ii) perceived effectiveness, (iii) intervention coherence, (iv) ethicality, and (v) self-efficacy, and disagreement with items reflecting (i) burden and (ii) opportunity costs
Our pre-registered criteria for inferring that owners found the pack acceptable (i.e., support for Hypothesis 3) was that the mean of items reflecting (i) affective attitudes, (ii) perceived effectiveness, (iii) intervention coherence, (iv) ethicality7, and (v) self-efficacy would be >3.5 (indicating agreement), while the mean of items reflecting (i) burden, and (ii) opportunity costs would be <2.5 (indicating disagreement). Table 6 shows the descriptive statistics (i.e., mean and standard deviations) for the measures of the acceptability of the health pack.
There was good evidence that owners found the health pack acceptable, in the sense that, on average, owners liked and enjoyed using the health pack (M = 3.89 on a 5-point scale, SD = 0.74), believed that it would be effective in helping them and other owners to manage their dogs weight (M = 3.99, SD = 0.68), and that it was clear how the health pack would do this (M = 4.44, SD = 0.80). Owners also reported feeling confident using the pack (M = 4.09, SD = 0.64), that using the pack was relatively easy (M = 4.01, SD = 0.97), did not require too much effort (M = 2.41, SD = 0.79) or interfere with their other priorities and / or make looking after their dog feel like a chore (M = 2.23, SD = 0.99). Owners also found the pack acceptable from an ethical perspective, in the sense that they agreed that it is okay to put a dog on a diet (M = 4.66, SD = 0.57) and did not feel that using the health pack made it difficult to show love for their dog (M = 1.66, SD = 0.91).
4.4 (exploratory) hypothesis 4: owners who are posted a health pack will report (i) changing the way that they feed, exercise, or interact with their dog over the 8 weeks following receipt of the pack, and (ii) these changes will be the result of receiving or using the health pack
Our pre-registered criteria for inferring Hypothesis 4 to be supported was that more than 70% of the owners who were posted a health pack would report (i) changing the way that they feed, exercise, or interact with their dog over the 8 weeks following receipt of the pack, and (ii) that these changes would result from receiving or using the health pack. 39 of the 49 participants (80%) who were posted a health pack and completed the follow-up questionnaire stated that they (or those in their household) changed the way that they fed, exercised, or interacted with their dog over the last 8 weeks. 36 of these participants (92%) stated that these changes were the result of receiving or using the health pack.
When asked to specify how their behavior had changed, 71% of the participants who were posted a health pack and completed the follow-up questionnaire reported changing the way that they feed (e.g., feeding smaller portions, less treats, or substituting treats for kibble or vegetables), 33% reported changing the amount or way that they exercise (e.g., more walks, throwing a ball in the park), and 51% reported changing the way that they interact with their dog (e.g., playing the games suggested by the Healthy Weight Cards, teaching tricks, or using enrichment toys like puzzles).
4.5 (exploratory) hypothesis 5: the weight and body condition score (BCS) of dogs will be lower at follow-up than at baseline
Our pre-registered criteria for inferring Hypothesis 5 to be supported was that the effect size reflecting the effect of time on (i) weight and (ii) BCS would be at least small (i.e., eta (2) > 0.01). We began by evaluating whether the data met the assumptions for the planned repeated measures ANOVA (i.e., no outliers, normally distributed, ratio-level data). Outliers were defined as values +/− 3SDs from the sample mean. At baseline, the average weight of the dogs was 19.10 kg (SD = 11.44), so we removed dogs weighing in excess of 53.42kgs (one dog: 60 kg8) from the estimate of baseline weight. At follow-up, the average weight of the dogs was 17.15 kg (SD = 9.81), defining outlying weights as those in excess of 46.58kgs. The heaviest dog at follow-up was reported to be 43.14kgs, so all values at follow-up were retained for analysis. The data on weight was positively skewed (baseline = 1.08, SE = 0.40, follow-up = 1.12, SE = 0.40) and so a square root transformation was applied prior to analysis to correct the skew (baseline = 0.73, SE = 0.38, follow-up = 0.74, SE = 0.40).
A repeated measures ANOVA revealed that the average weight of the dogs at baseline (M = 17.44, SD = 10.24) was higher than that at follow-up (M = 17.06, SD = 9.44), F (1, 33) = 4.30, p = 0.046. The effect size for this difference was small (eta (2) = 0.012). The data on BCS was ordinal level and so a non-parametric test was used to evaluate whether there was a difference in BCS between baseline (M = 5.70, SD = 1.14) and follow-up (M = 5.20, SD = 0.91).9 The Friedman’s test was statistically significant [chi-square (N = 47) = 16.67, p < 0.001]. The median BCS dropped from 6 at baseline to 5 at follow-up.
5 Discussion
The present research drew on behavioral science, insights from veterinary professionals, and feedback from owners to develop a health pack designed to support owners to manage the weight of their companion dogs. The pack targeted determinants of behavior specified by the COM-B model (54), including owners’ psychological capability (e.g., monitoring intake), physical capability (e.g., knowing how to weigh and score BCS), social opportunity (e.g., the behavior of others who may feed the dog), reflective motivation (e.g., awareness of the consequences of dogs being overweight), and automatic motivation (e.g.., pre-existing habits). This was achieved using 21 discrete behavior change techniques10 - many of which have been supported by extensive evidence (e.g., monitoring progress (65); action planning (51)), albeit primarily outside the veterinary context. Indeed, although not pre-planned, the health pack included a combination of behavior change techniques (namely, self-monitoring in addition to other techniques derived from control theory (66), such as goal setting) that evidence suggests is particularly effective in promoting healthy eating and physical activity in humans (67). That such findings translate to interventions designed to support dog owners to adopt similar behaviors in relation to their companion animals reiterates the potential of behavioral science in preventive veterinary medicine (22). It also speaks to the importance of using frameworks like the Behavior Change Intervention Ontology (62) to report interventions as so doing can help to build a cumulative evidence base in this context and contribute to broader debates about what behavioral interventions work, when, and for whom (68).
Phase 2 of the research evaluated whether the health pack was likely to be acceptable to owners and thus used, with the resulting changes in behavior. The findings supported this hypothesis. Over 90% of the owners who were posted a health pack and completed the follow-up questionnaire reported that they (and / or other members of their household) read or used parts of the pack. Although we did not measure how often or for how long participants used the materials, this finding is promising. One factor that likely contributed to the relatively high proportion of owners reporting using the pack is that owners found the health pack acceptable. That is, we found that owners typically liked and enjoyed using the health pack, believed that it would be effective in helping them and other owners to manage their dog’s weight (including talking to veterinary professionals about managing weight), and that it was clear how the health pack would do this. Owners also reported feeling confident using the pack, that using the pack was relatively easy and did not interfere with their other priorities and / or made looking after their dog feel like a chore. The finding that the pack was acceptable to owners is reassuring and, taken together with evidence that owners engaged with the materials, suggests that a printed health pack is a suitable way to deliver an intervention designed to support dog owners to manage the weight of their companion animals.
Although the primary purpose of the research reported in this paper was to evaluate the acceptability of the materials, we also explored potential effects on owners’ behavior and outcomes for their companion animals. The findings were encouraging – 80% of the owners who were posted a health pack and completed the follow-up questionnaire stated that they (or those in their household) changed the way that they fed, exercised, or interacted with their dog over the last 8 weeks - and the majority (92%) stated that these changes were the result of receiving or using the health pack. Notwithstanding some limitations (e.g., that the analyses are based on participants who completed the follow-up questionnaire – discussed further below), these are encouraging levels of compliance and stand in contrast with the relatively low levels of compliance reported with respect to other interventions. For example, evidence that just 21% of owners follow recommended therapeutic diets (38) and just 53% of owners follow physical activity recommendations (39). Although we did not expect to observe changes in weight and BCS (the study was not powered to detect such differences and the follow-up period was relatively short), there were indications that the weight and BCS of the dogs in the study improved. These findings need to be taken in the context of several limitations (below); however, they provide the basis for a full RCT to formally assess the effectiveness of the health pack against a control condition. Our suggestion would be that this trial measure continued as well as initial use of the pack and independently assess weight and BCS at a series of appropriate follow-up points (e.g., 3 and 6 months). The control condition could be standard veterinary advice (e.g., if the health pack was used to augment a consultation or nurse-led clinic).
5.1 Limitations
The findings of the present research need to be considered in the context of some limitations. First, 29 of the 78 participants (37%) who were posted a health pack did not complete the follow-up questionnaire. We tested our hypotheses by considering the responses of participants who completed the questionnaires; however, an alternative, more conservative test of Hypotheses 2 and 4 would be to assume that participants who did not complete the follow-up questionnaire did not use the pack (Hypothesis 2) or change the way that they feed, exercise, or interact with their dog (Hypothesis 4). Under this assumption (akin to an intention-to-treat analysis), neither hypothesis would be supported (i.e., 59% of owners who were posted a health pack report reported using the pack and 50% reported changing their behavior) and rates of compliance would be closer to estimates from other evaluations of interventions outside the laboratory (40). Attrition is a common problem in trials of interventions, particularly those delivered remotely (69) and there is debate as to how to handle missing data (70). However, future research should consider (i) further efforts to recontact participants who do not respond to identify if this is because (a) they have not used or liked the pack or (b) simply have not completed questionnaire (e.g., because they have not had time or have forgotten), and (ii) how to promote engagement and reduce attrition.
A second limitation of the present research was that weight and BCS were reported by owners rather than independently verified. Evidence suggests that owners’ typically underestimate their dogs’ BCS and weight (17, 18, 20). However, owner’s assessments are correlated with veterinary professionals’ assessments of BCS (r = 0.58 (20)) and the aim of our research was to evaluate change in weight from pre- to post-intervention. Therefore, although the present research may underestimate absolute levels of BCS, there is no reason to think that BCS would be underestimated to a greater extent at follow-up (indeed, given the instructions that owners received around assessing BCS in the health pack, we might expect the follow-up assessments to be more accurate and thus higher). Therefore, the estimation of change is likely more reliable than the absolute BCSs. Having said this, if the health pack were to be evaluated in a formal RCT with BCS as the primary outcome, it would be helpful to include more objective assessments, either directly by a veterinary professional or remotely. For example, Gant et al. (71) and Webb et al. (20) both found that it is possible to assess BCS from pictures that owners submit, albeit with the caveat that some owners struggle to take and submit appropriate pictures.
6 Conclusion
Overweight and obesity is a severe and prevalent problem among companion animals and there is a need for interventions that can support owners to make changes to their behavior. The present research shows that it is possible to develop materials to support owners to manage the weight of their companion animals that are likely to be used and may positively affect outcomes. The findings thus provide the basis for a full RCT to formally assess the effectiveness of the health pack against a control condition.
In addition to more formal evaluation of the effect of the pack on outcomes, future research could also consider how the pack might be used. The tools were designed to be used by owners independently of veterinary professionals. However, it may be necessary to check that it is appropriate to limit food intake (e.g., via a brief – remote if needed – consult to check the health status of the dog, as in the present research) prior to owners doing so. If so, future research could also evaluate potential ways to provide this check – e.g., online decision tools supported by AI, in person or remote consult, with a vet nurse or trained staff at, for example, a pet store. Alternatively, or in addition, the pack might be used to support veterinary professionals to work with owners. For example, the pack could provide resources for owners to take home after a veterinary consultation. This approach would fit with owner’s feedback on the initial set of tools, which suggested that some degree of personalisation would be helpful to ensure that the tools work for different dogs and households. Owners also felt that the pack would help them to discuss weight management with professionals. In this sense, the tools might facilitate conversations around weight that many veterinarians find difficult (32).
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: Open Science Framework: https://doi.org/10.17605/OSF.IO/D9ZTP.
Ethics statement
The studies involving humans were approved by the Research Ethics Committee, the University of Sheffield. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
TW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Methodology, Project administration, Supervision, Writing – original draft, Writing – review & editing. JM: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Writing – review & editing. LS: Conceptualization, Methodology, Writing – review & editing. HP: Conceptualization, Funding acquisition, Methodology, Project administration, Resources, Supervision, Writing – review & editing. JB: Data curation, Formal analysis, Investigation, Methodology, Writing – original draft. HA: Data curation, Formal analysis, Investigation, Writing – review & editing. OM: Methodology, Writing – review & editing. SM: Data curation, Investigation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This work was funded by Nestlé Purina PetCare.
Acknowledgments
The authors are grateful to Meghann Matthews for help describing the health pack using the COM-B model and Behavior Change Intervention Ontology.
Conflict of interest
Thomas L. Webb reports a relationship with Nestle Purina Petcare that includes consulting, funding, and speaking and lecture fees.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fvets.2024.1483130/full#supplementary-material
Footnotes
1. ^Receptionists were included because, although not trained in veterinary medicine, they often have good relationships with patients and the time spent talking may help to identify some of the more everyday experiences of dog owners.
2. ^Potential participants were provided with a BCS chart to facilitate this assessment and were also asked to submit a photo of their dog to allow some initial verification by the research team.
3. ^We recognise that weight in itself is not a measure of overweight / obesity – hence the inclusion of BCS. However, owners needed to be willing and able to weigh their dogs to benefit from some tools in the health pack (e.g., the weight loss progress chart) and this data allowed us to evaluate changes in weight as a secondary outcome (Hypothesis 5).
4. ^Participants were also asked to complete measures of beliefs specified by Protection Motivation Theory (64) using items from our previous research (20). This included measures of (i) threat appraisal – severity (“Overweight and obesity cause severe problems in dogs” and “The health risks associated with overweight and obesity in dogs are severe”), (ii) threat appraisal – vulnerability (“The chances are high that my dog is, or will become, overweight” and “My dog easily puts on weight”), (iii) coping appraisal - response efficacy (“Ensuring my dog is the correct weight will help to reduce health problems” and “Ensuring my dog is the correct weight will mean that they have a long and healthy life”), and (iv) coping appraisal - self-efficacy (“I am capable of keeping my dog at a healthy weight” and “I am capable of helping my dog to lose weight if needed”). These items were not part of the pre-registered analyses and so are not reported further.
5. ^Our pre-registered aim was to recontact owners eight weeks (56 days) after posting the pack, but a number of logistical challenges, including the Christmas vacation meant that owners were recontacted slightly later than planned.
6. ^This estimate excludes one outlying weight (60 kg) as described in the analysis of Hypothesis 5. We also removed the weight data for one participant as the increase in weight was improbable (a chihuahua which was reported to weigh 4 kg at baseline, but 20 kg at follow-up).
7. ^Note that this hypothesis was pre-registered as predicting disagreement with items reflecting ethicality. However, the questions were coded such that high scores indicated that owners viewed the health pack as a good fit with their value system (e.g., that they agreed that “it is okay to put a dog on a diet”) and so agreement with these items indicated that the health pack was acceptable to owners.
8. ^The owner did not report the weight of this dog at follow-up.
9. ^Note that the use of a non-parametric test represents a deviation from the pre-registration which specified that a second repeated measures repeated measures ANOVA would be used to examine changes in BCS as a function of time. However, the planned analysis neglected to account for the fact that BCS is an ordinal-level variable.
10. ^Some behavior change techniques were delivered by more than one component of the intervention. For example, both the weight loss progress chart and monthly milestones chart prompted owners to self-monitor the outcomes of their behavior (BCIO:007025).
References
1. O’Neill, DG, James, H, Brodbelt, DC, Church, DB, and Pegram, C. Prevalence of commonly diagnosed disorders in UK dogs under primary veterinary care: results and applications. BMC Vet Res. (2021) 17:69. doi: 10.1186/s12917-021-02775-3
2. Association for Pet Obesity Prevention (APOP). Pet obesity prevalence survey and pet owner: weight management, nutrition, and pet food survey. (2018). Available at: https://www.petobesityprevention.org/2018 (Accessed December 3, 2024).
3. World Health Organization. Obesity and overweight. (2024). Available at: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight (Accessed December 3, 2024).
4. Henegar, JR, Bigler, SA, Henegar, LK, Tyagi, SC, and Hall, JE. Functional and structural changes in the kidney in the early stages of obesity. J Am Soc Nephrol. (2001) 12:1211–7. doi: 10.1681/ASN.V1261211
5. Liu, DJX, Stock, E, Broeckx, BJG, Daminet, S, Meyer, E, Delanghe, JR, et al. Weight-gain induced changes in renal perfusion assessed by contrast-enhanced ultrasound precede increases in urinary protein excretion suggestive of glomerular and tubular injury and normalize after weight-loss in dogs. PLoS One. (2020) 15:e0231662. doi: 10.1371/journal.pone.0231662
6. McCarthy, PMG, Whittaker, CJ, Annear, MJ, Hall, E, Hamzianpour, N, Irving, W, et al. Parasiticide use and obesity in dogs with sudden acquired retinal degeneration syndrome. J Am Vet Med Assoc. (2024) 262:1–6. doi: 10.2460/javma.24.02.0140
7. Raffan, E, Smith, SP, O’Rahilly, S, and Wardle, J. Development, factor structure and application of the dog obesity risk and appetite (DORA) questionnaire. Peer J. (2015) 3:e1278. doi: 10.7717/peerj.1278
8. German, AJ, Holden, SL, Wiseman-Orr, ML, Reid, J, Nolan, AM, Biourge, V, et al. Quality of life is reduced in obese dogs but improves after successful weight loss. Br Vet J. (2012) 192:428–34. doi: 10.1016/j.tvjl.2011.09.015
9. Yam, PS, Butowski, CF, Chitty, JL, Naughton, G, Wiseman-Orr, ML, Parkin, T, et al. Impact of canine overweight and obesity on health-related quality of life. Prev Vet Med. (2016) 127:64–9. doi: 10.1016/j.prevetmed.2016.03.013
10. Flanagan, J, Bissot, T, Hours, MA, Moreno, B, Feugier, A, and German, AJ. Success of a weight loss plan for overweight dogs: the results of an international weight loss study. PLoS One. (2017) 12:e0184199. doi: 10.1371/journal.pone.0184199
11. Kealy, RD, Lawler, DF, Ballam, JM, Mantz, SL, Biery, DN, Greeley, EH, et al. Effects of diet restriction on life span and age-related changes in dogs. J Am Vet Med Assoc. (2002) 220:1315–20. doi: 10.2460/javma.2002.220.1315
12. Salt, C, Morris, PJ, Wilson, D, Lund, EM, and German, AJ. Association between life span and body condition in neutered client-owned dogs. J Vet Intern Med. (2019) 33:89–99. doi: 10.1111/jvim.15367
13. German, AJ. The growing problem of obesity in dogs and cats. J Nutr. (2006) 136:1940S–6S. doi: 10.1093/jn/136.7.1940S
14. Pegram, C, Raffan, E, White, E, Ashworth, AH, Brodbelt, DC, Church, DB, et al. Frequency, breed predisposition and demographic risk factors for overweight status in dogs in the UK. J Small Anim Pract. (2021) 62:521–30. doi: 10.1111/jsap.13325
15. Webb, TL. Why pet owners overfeed: a self-regulation perspective. Paper presented at the Nestlé Purina companion animal nutrition summit on “pet obesity: the future of weight management”. (2015).
16. Eastland-Jones, RC, German, AJ, Holden, SL, Biourge, V, and Pickavance, LC. Owner misperception of canine body condition persists despite use of a body condition score chart. J Nutr Sci. (2014) 3:e45. doi: 10.1017/jns.2014.25
17. White, GA, Hobson-West, P, Cobb, K, Craigon, J, Hammond, R, and Millar, KM. Canine obesity: is there a difference between veterinarian and owner perception? J Small Anim Pract. (2011) 52:622–6. doi: 10.1111/j.1748-5827.2011.01138.x
18. Muñoz-Prieto, A, Nielsen, LR, Dąbrowski, R, Bjørnvad, CR, Söder, J, Lamy, E, et al. European dog owner perceptions of obesity and factors associated with human and canine obesity. Sci Rep. (2018) 8:13353. doi: 10.1038/s41598-018-31532-0
19. Webb, TL, du Plessis, H, Christian, H, Raffan, E, Rohlf, V, and White, GA. Understanding obesity among companion dogs: new measures of owner’s beliefs and behaviour and associations with body condition scores. Prev Vet Med. (2020) 180:105029. doi: 10.1016/j.prevetmed.2020.105029
20. Chan, CB, Spierenburg, M, Ihle, SL, and Tudor-Locke, C. Use of pedometers to measure physical activity in dogs. JAVMA. (2005) 226:2010–5. doi: 10.2460/javma.2005.226.2010
21. Nielson, SA, Khosa, DK, Clow, KM, and Verbrugghe, A. Dog caregivers’ perceptions, motivations, and behaviours for feeding treats: a cross sectional study. Prev Vet Med. (2023) 217:105971. doi: 10.1016/j.prevetmed.2023.105971
22. Webb, TL. Interview in new perspectives on pet obesity: moving to a behavioural science model. Purina (2022). Available at: https://www.vettimes.co.uk/purina-obesity-ebook/
23. Kienzle, E, Bergler, R, and Mandernach, A. A comparison of the feeding behavior and the human-animal relationship in owners of normal and obese dogs. J Nutr. (1998) 128:S2779–82. doi: 10.1093/jn/128.12.2779S
24. Morelli, G, Marchesini, G, Contiero, B, Fusi, E, Diez, M, and Ricci, R. A survey of dog owners’ attitudes toward treats. J Appl Anim Welf Sci. (2019) 23:1–9. doi: 10.1080/10888705.2019.1579095
25. White, GA, Ward, L, Pink, C, Craigon, J, and Millar, KM. “Who’s been a good dog?” – owner perceptions and motivations for treat giving. Prev Vet Med. (2016) 132:14–9. doi: 10.1016/j.prevetmed.2016.08.002
26. Borne, AT, Wolfsheimer, KJ, Truett, AA, Kiene, J, Wojciechowski, T, Davenport, DJ, et al. Differential metabolic effects of energy restriction in dogs using diets varying in fat and fiber content. Obes Res. (1996) 4:337–45. doi: 10.1002/j.1550-8528.1996.tb00241.x
27. Diez, M, Jeusette, I, Istasse, L, Nguyen, P, Devois, C, and Biourge, V. Weight loss in obese dogs: evaluation of a high-protein, low-carbohydrate diet. J Nutr. (2002) 132:1685S–7S. doi: 10.1093/jn/132.6.1685S
28. Laflamme, DP, and Kuhlman, G. The effect of weight loss regimen on subsequent weight maintenance in dogs. Nutr Res. (1995) 15:1019–28. doi: 10.1016/0271-5317(95)00063-O
29. Saker, KE, and Remillard, RL. Performance of a canine weight-loss program in clinical practice. Vet Ther. (2005) 6:291–302.
30. Ackerman, N. Nurse-led obesity clinics: facilitating weight loss in dogs and cats. Veterinary Nur. (2012) 3:570–3. doi: 10.12968/vetn.2012.3.9.570
31. Shutt, J. Pet obesity – lightening the load with vet nurse-led weight clinics. Vet Times. (2023) 23:12–3.
32. Aldewereld, CM, Monninkhof, EM, Kroese, FM, de Ridder, DTD, Nielen, M, and Corbee, RJ. Discussing overweight in dogs during a regular consultation in general practice in the Netherlands. J Anim Physiol Anim Nutr. (2021) 105:56–64. doi: 10.1111/jpn.13558
33. Pearl, RL, Wadden, TA, Bach, C, Leonard, SM, and Michel, KE. Who’s a good boy? Effects of dog and owner body weight on veterinarian perceptions and treatment recommendations. Int J Obes. (2020) 44:2455–64. doi: 10.1038/s41366-020-0622-7
34. Sutherland, KA, Coe, JB, Janke, N, O’Sullivan, TL, and Parr, JM. Pet owners’ and companion animal veterinarians’ perceptions of weight-related veterinarian-client communication. J Am Vet Med Assoc. (2022) 260:1697–703. doi: 10.2460/javma.22.03.0101
35. Sutherland, KA, Coe, JB, and O’Sullivan, TL. Exploring veterinary professionals’ perceptions of pet weight-related communication in companion animal veterinary practice. Vet Record. (2023) 192:e 1973. doi: 10.1002/vetr.1973
36. MacMartin, C, Wheat, H, and Coe, JB. Conversation analysis of clients’ active resistance to veterinarians’ proposals for long-term dietary change in companion animal practice in Ontario, Canada. Animals. (2023) 13:2150. doi: 10.3390/ani13132150
37. Carciofi, AC, Gonçalves, KNV, Vasconcellos, RS, Bazolli, RS, Brunetto, MA, and Prada, F. A weight loss protocol and owners participation in the treatment of canine obesity. Ciência Rural. (2005) 35:1331–8. doi: 10.1590/S0103-84782005000600016
38. American Animal Hospital Association. The path to high quality care: Practical tips for improving compliance. Lakewood, CO: AAHA Press (2003).
39. Porsani, MYH, Teixeira, FA, Amaral, AR, Pedrinelli, V, Vasques, V, de Oliveira, AG, et al. Factors associated with failure of dog’s weight loss programmes. Vet Med Sci. (2019) 6:299–305. doi: 10.1002/vms3.229
40. German, AJ, Titcomb, JM, Holden, SL, Queau, Y, Morris, PJ, and Biourge, V. Cohort study of the success of controlled weight loss programs for obese dogs. J Vet Intern Med. (2015) 29:1547–55. doi: 10.1111/jvim.13629
41. Krasuska, M, and Webb, TL. How effective are interventions designed to help owners to change their behaviour so as to manage the weight of their companion dogs? A systematic review and meta-analysis. Prev Vet Med. (2018) 159:40–50. doi: 10.1016/j.prevetmed.2018.08.016
42. Yaissle, JE, Holloway, C, and Buffington, CAT. Evaluation of owner education as a component of obesity treatment programs for dogs. J Am Vet Med Assoc. (2004) 224:1932–5. doi: 10.2460/javma.2004.224.1932
43. Banton, S, von Massow, M, Pezzali, JG, Verbrugghe, A, and Shoveller, AK. Jog with your dog: dog owner exercise routines predict dog exercise routines and perception of ideal body weight. PLoS One. (2022) 17:e0272299. doi: 10.1371/journal.pone.0272299
44. Byers, CG, Wilson, CC, Stephens, MB, Goodie, JL, Netting, FE, and Olsen, CH. Owners and pets exercising together: canine response to veterinarian-prescribed physical activity. Anthrozoös. (2014) 27:325–33. doi: 10.2752/175303714X14036956449224
45. Morrison, R, Reilly, JJ, Penpraze, V, Westgarth, C, Ward, DS, Mutrie, N, et al. Children, parents and pets exercising together (CPET): exploratory randomised controlled trial. BMC Public Health. (2013) 13:1096. doi: 10.1186/1471-2458-13-1096
46. Wakshlag, JJ, Struble, AM, Warren, BS, Maley, M, Panasevich, MR, Cummings, KJ, et al. Evaluation of dietary energy intake and physical activity in dogs undergoing a controlled weight-loss program. J Am Vet Med Assoc. (2012) 240:413–9. doi: 10.2460/javma.240.4.413
47. Chauvet, A, Laclair, J, Elliott, DA, and German, AJ. Incorporation of exercise, using an underwater treadmill, and active client education into a weight management program for obese dogs. Can Vet J. (2011) 52:491–6.
48. Webb, TL, Krasuska, M, Toth, Z, du Plessis, HR, and Colliard, L. Using research on self-regulation to understand and tackle the challenges that owners face helping their (overweight) dogs to lose weight. Prev Vet Med. (2018) 159:227–31. doi: 10.1016/j.prevetmed.2018.08.017
49. Armitage, CJ. A volitional help sheet to encourage smoking cessation: a randomized exploratory trial. Health Psychol. (2008) 27:557–66. doi: 10.1037/0278-6133.27.5.557
50. Gollwitzer, PM. Implementation intentions: strong effects of simple plans. Am Psychol. (1999) 54:493–503. doi: 10.1037/0003-066X.54.7.493
51. Sheeran, P, Listrom, O, and Gollwitzer, PM. The when and how of planning: Meta-analysis of the scope and components of implementation intentions in 642 tests. Eur rev. Soc Psychol. (2024):1–33. doi: 10.1080/10463283.2024.2334563
52. Sekhon, M, Cartwright, M, and Francis, JJ. Acceptability of healthcare interventions: an overview of reviews and development of a theoretical framework. BMC Health Serv Res. (2017) 17:88. doi: 10.1186/s12913-017-2031-8
53. Prestwich, A, Webb, TL, and Conner, MT. Using theory to develop and test interventions to promote changes in health behaviour: evidence, issues, and recommendations. Curr Opin Psychol. (2015) 5:1–5. doi: 10.1016/j.copsyc.2015.02.011
54. Michie, S, van Stralen, MM, and West, R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. (2011) 6:42. doi: 10.1186/1748-5908-6-42
55. Sheeran, P, and Webb, TL. The intention–behavior gap. Soc Personal Psychol Compass. (2016) 10:503–18. doi: 10.1111/spc3.12265
56. Webb, TL, and Sheeran, P. Does changing behavioral intentions engender behavior change? A meta-analysis of the experimental evidence. Psychol Bull. (2006) 132:249–68. doi: 10.1037/0033-2909.132.2.249
57. Biesheuvel, MM, Santman-Berends, IMGA, Barkema, HW, Ritter, C, Berezowski, J, Guelbenzu, M, et al. Understanding farmers’ behavior and their decision-making process in the context of cattle diseases: a review of theories and approaches. Front Vet Sci. (2021) 8:8. doi: 10.3389/fvets.2021.687699
58. Farrell, S, Benson, T, McKernan, C, Regan, A, Burrell, AMG, and Dean, M. Factors influencing dairy farmers’ antibiotic use: an application of the COM-B model. J Dairy Sci. (2023) 106:4059–71. doi: 10.3168/jds.2022-22263
59. Farrell, S, Benson, B, McKernan, C, Regan, A, Burrell, AMG, and Dean, M. Exploring veterinarians’ behaviour relating to antibiotic use stewardship on Irish dairy farms using the COM-B model of behaviour change. Res Vet Sci. (2023) 156:45–53. doi: 10.1016/j.rvsc.2023.01.019
60. Furtado, T, Perkins, E, Pinchbeck, G, McGowan, C, Watkins, F, and Christley, R. Exploring human behavior change in equine welfare: insights from a COM-B analysis of the UK’s equine obesity epidemic. Front Vet Sci. (2022) 9:9. doi: 10.3389/fvets.2022.961537
61. Marques, MM, Wright, AJ, Corker, E, Johnston, M, West, R, Hastings, J, et al. The behaviour change technique ontology: transforming the behaviour change technique taxonomy v1. Wellcome Open Res. (2024) 8:308. doi: 10.12688/wellcomeopenres.19363.2
62. Michie, S, West, R, Finnerty, AN, Norris, E, Wright, AJ, Marques, MM, et al. Representation of behaviour change interventions and their evaluation: development of the upper level of the behaviour change intervention ontology. Wellcome Open Res. (2021) 5:123. doi: 10.12688/wellcomeopenres.15902.2
63. Ben-Zeev, D, Brenner, CJ, Begale, M, Duffecy, J, Mohr, DC, and Mueser, KT. Feasibility, acceptability, and preliminary efficacy of a smartphone intervention for schizophrenia. Schizophr Bull. (2014) 40:1244–53. doi: 10.1093/schbul/sbu033
64. Maddux, JE, and Rogers, RW. Protection motivation and self-efficacy: a revised theory of fear appeals and attitude change. J Exp Soc Psychol. (1983) 19:469–79. doi: 10.1016/0022-1031(83)90023-9
65. Harkin, B, Webb, TL, Chang, BPI, Prestwich, A, Conner, MT, Kellar, I, et al. Does monitoring goal progress promote goal attainment? A meta-analysis of the experimental evidence. Psychol Bull. (2016) 142:198–229. doi: 10.1037/bul0000025
66. Carver, CS, and Scheier, MF. Control theory: a useful conceptual framework for personality–social, clinical, and health psychology. Psychol Bull. (1982) 92:111–35. doi: 10.1037/0033-2909.92.1.111
67. Michie, S, Abraham, C, Whittington, C, McAteer, J, and Gupta, S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. (2009) 28:690–701. doi: 10.1037/a0016136
68. Michie, S, Thomas, J, Johnston, M, Aonghusa, PM, Shawe-Taylor, J, Kelly, MP, et al. The human behaviour-change project: harnessing the power of artificial intelligence and machine learning for evidence synthesis and interpretation. Implement Sci. (2017) 12:121. doi: 10.1186/s13012-017-0641-5
69. Meyerowitz-Katz, G, Ravi, S, Arnolda, L, Feng, X, Maberly, G, and Astell-Burt, T. Rates of attrition and dropout in app-based interventions for chronic disease: systematic review and meta-analysis. J Med Internet Res. (2020) 22:e20283. doi: 10.2196/20283
70. Andrade, C. Intent-to-treat (ITT) vs completer or per-protocol analysis in randomized controlled trials. Indian J Psychol Med. (2022) 44:416–8. doi: 10.1177/02537176221101996
Keywords: obesity, overweight, weight management, dog, owner, behavioral science, COM-B model
Citation: Webb TL, Molina J, Sheridan L, du Plessis H, Brown J, Abraham H, Morton O and McKay S (2025) Developing and evaluating a health pack to support dog owners to manage the weight of their companion animals. Front. Vet. Sci. 11:1483130. doi: 10.3389/fvets.2024.1483130
Edited by:
Daniel Mota-Rojas, Metropolitan Autonomous University, MexicoReviewed by:
Adriana Olmos-Hernández, National Institute of Rehabilitation Luis Guillermo Ibarra Ibarra, MexicoKarina Lezama, Universidad Autónoma Metropolitana, Mexico
Copyright © 2025 Webb, Molina, Sheridan, du Plessis, Brown, Abraham, Morton and McKay. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thomas L. Webb, dC53ZWJiQHNoZWZmaWVsZC5hYy51aw==
 Thomas L. Webb
Thomas L. Webb Jenifer Molina2
Jenifer Molina2